White Potatoes & Resistant Starch: A Surprising Ally for Gut Health and Histamine Intolerance
White potatoes might not be the trendy superfood on everyone’s plate, but don’t let their simplicity fool you. When cooked and cooled, these everyday tubers are packed with a special kind of fiber called resistant starch. Once it reaches your colon, it fuels good gut bacteria. It boosts production of butyrate—a powerful short-chain fatty acid (SCFA) known to reduce inflammation, improve gut lining integrity, and even dial down histamine reactions. If you’ve been told to fear carbs or ditch potatoes, it’s time to rethink that advice—your gut may actually thank you.
One of my favorite foods has always been French fries—a totally low-histamine food that has always been an indulgence for me. But now I have learned to enjoy my fries on an occasional basis, knowing that they are good for the gut and help produce butyrate, lowering histamine release by the mast cells.
Let's Talk Resistant Starch & Histamine Intolerance
Resistant starch (RS) is a type of carbohydrate that resists digestion in the small intestine. Instead of breaking down like regular carbs, RS travels to the colon, where gut bacteria ferment it into beneficial compounds, particularly SCFAs such as acetate, propionate, and butyrate.
Not all fiber is created equal. There are several types:
Soluble fiber easily dissolves in water and can help lower blood sugar and cholesterol. A standard soluble fiber is psyllium (corn or rice).
Insoluble fiber does not dissolve in water and adds bulk to stool, supporting regularity.
Prebiotic fiber is fiber that we cannot digest and instead helps feed beneficial gut microbes.
And resistant starch, which uniquely behaves like fiber and a prebiotic.
Resistant starch acts like fertilizer for your gut. When fermented, it creates SCFAs, with butyrate being the standout. Why? Because it’s the favorite fuel for your colon cells, which are responsible for helping to support a healthy microbiota, maintaining the integrity of our gut lining, and supporting a balanced immune response. Our colon cells play a crucial role in helping to reduce histamine release, enabling us to tolerate foods that are high in histamine.
The Benefits of SCFAs (Especially Butyrate)
Once your colon bacteria break down resistant starch, the SCFAs kick off a host of health benefits:
- Immune Cell Regulation: Butyrate helps balance immune responses, keeping overreactions (like those involved in
histamine intolerance and autoimmune flare-ups) in check. - Anti-inflammatory Power: It calms inflammation in the gut and throughout our whole body. That’s especially important if you're prone to food reactions or skin flare-ups.
- Epigenetic Support: Butyrate influences gene expression by modulating histone deacetylase (HDAC) activity, which has ripple effects on inflammation, immunity, and even mental health.
- Stronger Gut Barrier: It reinforces the gut lining, preventing leaky gut—a condition tied to food intolerances, fatigue, brain fog, and histamine overload.
- Support Beyond the Gut: Studies show SCFAs help calm immune responses in the lungs and skin, reducing asthma symptoms and even atopic dermatitis.
What Happens When Fiber Intake Is Too Low?
A low-fiber, high-fat diet—common in the Western world—is a recipe for gut imbalance. Not only is it lacking in key nutrients like vitamins and polyphenols, but it also reduces the production of short-chain fatty acids (SCFAs), especially butyrate, which starves the cells lining your colon.
This type of diet disrupts the gut microbiota, promoting the growth of inflammatory bacteria, such as Proteobacteria, and reducing the fermentation of microbes that produce short-chain fatty acids (SCFAs).
It can also interfere with gene expression involved in maintaining oxygen balance in the gut, leading to bacterial overgrowth and increased production of endotoxins such as lipopolysaccharides (LPS), which fuel inflammation and trigger histamine release.
On top of that, it lowers the activity of the DAO enzyme, making it harder for your body to break down histamine and increasing your sensitivity to high-histamine foods. Together, these effects create a domino effect that worsens
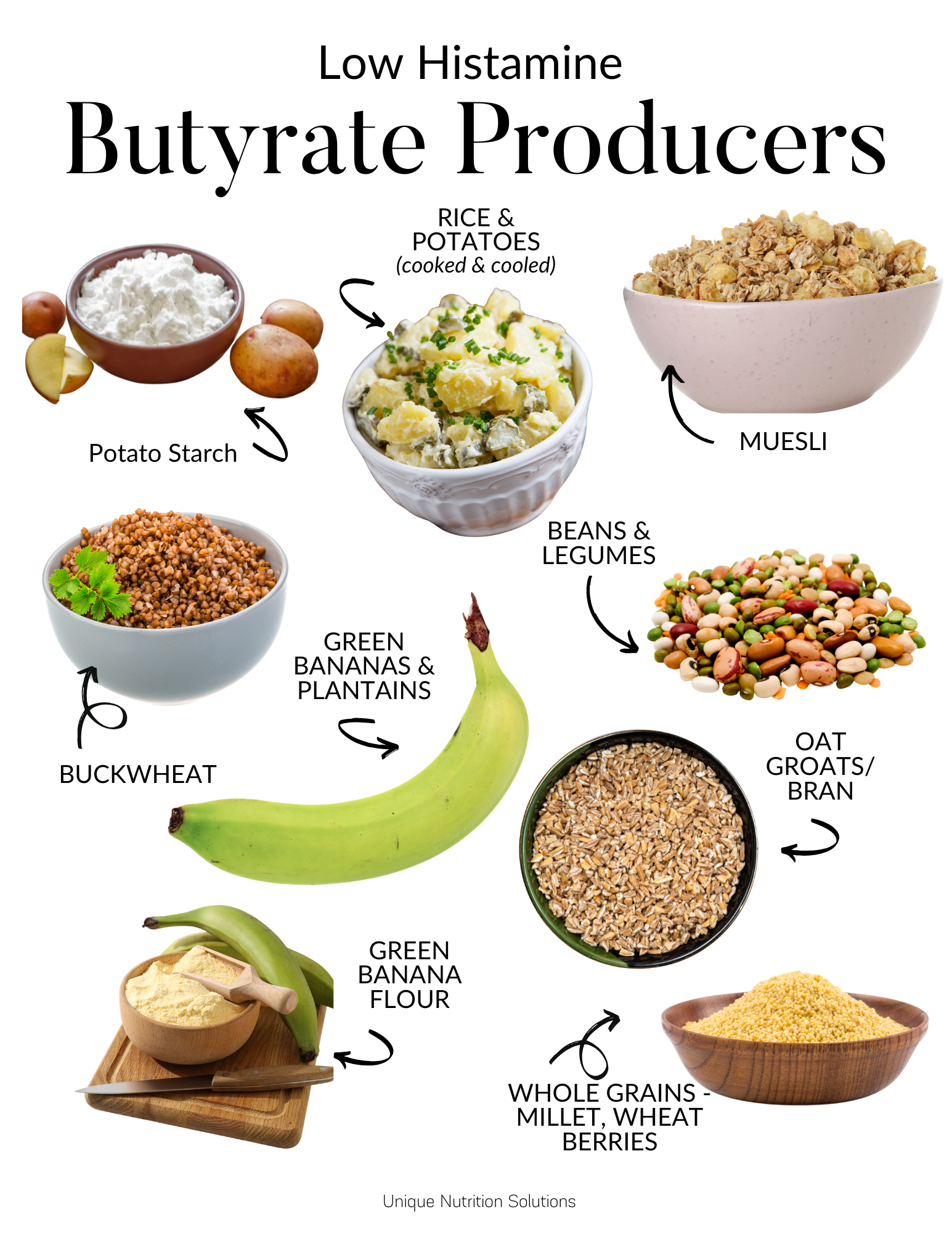
Best Low Histamine Sources of Resistant Starch
If you’re ready to show your gut some love, start with these:
- White Potatoes (especially cooked and cooled)
- Green Banana Flour
- Legumes (like lentils and chickpeas)
- Oats and Brown rice
Note: Raw white potatoes contain the most resistant starch, but they’re unsafe to eat raw because they contain natural toxins like solanine and lectins, which make them difficult to digest. Stick to cooked and cooled methods, such as potato salad.
Can You Boost RS by Cooking Differently?
One simple and effective way to increase resistant starch in your meals is to cook and then cool starch-rich foods, a process known as retrogradation. When starchy foods, such as potatoes, rice, or legumes, are cooked and allowed to cool, some of their starches convert into a form that resists digestion—resistant starch. Dishes such as potato salad, cold rice bowls, or lentil salads are great examples.
While the exact amount of resistant starch formed can vary and is still a topic of debate in research, both anecdotal evidence and mechanisms suggest that this method is beneficial.
It's worth noting that sweet potatoes, although nutritious, naturally contain lower levels of resistant starch and aren’t the best choice if your main goal is boosting butyrate.
Interestingly, pressure cooking has been shown to reduce resistant starch levels, yet it remains a convenient option for preparing foods like potatoes, legumes, and oat groats. For tougher grains like oat groats or wheat berries, which are naturally higher in resistant starch, using a pressure cooker or an Instant Pot can significantly cut down cooking time without sacrificing too much of their beneficial content.
Green Bananas: A Double Win for Histamine Intolerance
Green bananas are rich in resistant starch and low in sugar and histamine—making them a great option for those with
Bonus Tip: Green banana flour is a supplement option. Just be cautious—it's high in tryptophan, which could potentially affect serotonin levels if you’re already dealing with mood or anxiety issues.
Best Resistant Starch Supplement for Histamine Intolerance
PaleoFiber® RS is a unique resistant starch supplement that goes beyond basic fiber by combining organic green banana flour, organic potato starch, and prebiotic fibers like arabinogalactan from larch trees. This thoughtful blend fuels beneficial gut bacteria, promoting the natural production of short-chain fatty acids (SCFAs) like butyrate, which support a healthy gut lining, balanced immune response, and improved metabolism.
Unlike other resistant starch powders that rely solely on potato starch, this formula incorporates green banana flour—a rich source of nutrients like potassium and polyphenols—and cellulose, thereby enhancing the production of butyrate.
Together, these ingredients work synergistically to support gut integrity, encourage microbial diversity, balance immune response, and nourish the colon cells. Ideal for mixing into smoothies or yogurt, this powder provides an easy and natural way to boost fiber intake and support your body’s internal ecosystem.
Join my Fullscript Account and get access to my Best Fiber for Healthy Gut and Histamine Intolerance Guide. Get 15% off DFH, PaleoRS, and free shipping on orders over $50.00!
Can You Supplement with Butyrate?
If antibiotics, stress, or illness have disrupted your gut microbiome and depleted your butyrate-producing bacteria, supporting your gut with tributyrin may be a smart step. Tributyrin is a highly absorbable, stable form of butyrate—an essential short-chain fatty acid that fuels colon cells, reduces inflammation, and supports gut lining repair.
Unlike standard probiotics, tributyrin doesn’t require live bacteria to be effective, making it a reliable option after antibiotic use. Recent research suggests that taking probiotics either concurrently with an antibiotic or shortly after completing treatment may slow down the recovery of your gut's microbiota. It is now recommended to wait 3-5 months. However, tributyrin has been shown to help heal the gut quickly and support colon cells, thereby reducing histamine overload.
Tributyrin enhances energy production in colonocytes, rebalances oxygen levels in the gut to prevent harmful bacterial overgrowth, and reduces excess histamine, a significant benefit for individuals with sensitivities. It also activates genes, such as HIF-1α, which help regulate energy use and maintain gut integrity. Look for products like TributyrinX from Healthy Gut, which deliver butyrate in its triglyceride form to improve stability and absorption. This makes it a more efficient way to support gut health, especially when you're recovering from microbiome disruptions.
Are There Genes That Influence Fiber Needs?
Absolutely. Some gene variants can raise your body’s need for resistant starch and fiber. These include:
- FUT2 – Affects gut microbiota composition and response to prebiotics.
- SLC22A5 – Linked to mitochondrial energy and butyrate transport that increases your demand for L-carnitine.
- DAO – Directly tied to your ability to break down histamine
- PPAR-Gamma – Regulates colonocyte metabolism and gut barrier function.
- HIF1-Alpha – Critical for oxygen balance and gut homeostasis
Understanding your unique genetic blueprint can help tailor your fiber and supplement choices for better gut and immune health. If you want to learn more about these genes and if you have these variants, check out my Histamine Genes programs.
Bottom Line
White potatoes may not wear a “superfood” cape, but don’t underestimate their power, especially when cooled. Their resistant starch content can help produce more butyrate, balance your gut, and improve your body’s ability to handle histamine.
Instead of fearing carbs, start thinking about how you can work with your food to heal your gut and regulate your immune system. Sometimes, health-supportive foods aren’t exotic—they’re right in your kitchen. Want to learn more about how to cook low-histamine? Check out my Cooking Low Histamine program.
References
- Eroglu, E. I., & Buyuktuncer, Z. (2017). The effect of various cooking methods on resistant starch content of foods. Nutrition & Food Science, 47(4), 522–533. https://doi.org/10.1108/NFS-10-2016-0154
- Folkerts, J., Stadhouders, R., Redegeld, F. A., Tam, S.-Y., Hendriks, R. W., Galli, S. J., & Maurer, M. (2018). Effect of dietary fiber and metabolites on mast cell activation and mast cell-associated diseases. Frontiers in Immunology, 9, 1067. https://doi.org/10.3389/fimmu.2018.01067
- Litvak, Y., Byndloss, M. X., & Bäumler, A. J. (2018). Colonocyte metabolism shapes the gut microbiota. Science, 362(6418), eaat9076. https://doi.org/10.1126/science.aat9076
- Pral, L. P., Fachi, J. L., Corrêa, R. O., Colonna, M., & Vinolo, M. A. R. (2021). Hypoxia and HIF-1 as key regulators of gut microbiota and host interactions. Trends in Immunology, 42(7), 604–621. https://doi.org/10.1016/j.it.2021.05.004







