What is Histamine Intolerance?
Does it seem like every time you have a glass of wine and a cheese appetizer, you get a headache or even a migraine a few hours later? You might have histamine intolerance.
Both cheese and wine, especially red wine, are high in histamine, a chemical produced during the fermentation process of making wine and cheese.
You are probably more familiar with histamine as a chemical released by the body with allergic reactions like sneezing, watery eyes, and skin rashes. And that is why you reach for antihistamine medications like Zyrtec, Claritin, or maybe Benadryl.
Histamine levels can reach toxic levels from foods high in histamine, a biogenic amine, or from what your body produces due to poor degradation or breakdown of histamine and its cousin, tyramine.
Biogenic amines are a group of protein compounds that the body produces or are formed in foods mostly during the fermentation process. Other biogenic amines predominately found in food are putrescine and cadaverine.
All biogenic amines can cause a toxic reaction if levels are too high, with histamine and tyramine having the highest potential to lead to symptoms of food poisoning.
Histamine intoxication was first described over 60 years ago when ingestion of fish from the scombroid family which includes tuna fish caused rash, diarrhea, reddening or flushing of the face and sometimes the neck, arms, and upper part of the body, sweating, headache, and vomiting.
Other fish that are in the scombroid family are tuna fish, mackerel, skipjack, and bonito and can form high levels of histamine if left in higher temperatures or not properly stored.
Recently however, it has been discovered that high levels of histamine usually caused by lack of enzymes like diamine oxidase (DAO) and histamine methyltransferase (HNMT) to degrade histamine, can lead to the symptoms of histamine intoxication or histamine intolerance.
How Can You Become Toxic with Histamine?
Two main enzymes, DAO and HNMT, help break down histamine so that our bodies can safely eliminate histamine. The DAO enzyme also breakdowns other biogenic amines, putrescine, and cadaverine; however, DAO prefers histamine.
DAO is found predominantly in the gastrointestinal tract and degrades and blocks histamine from our food, playing a significant role in keeping histamine and biogenic amines at safe levels.
HNMT, on the other hand, plays a lesser role in the degradation of histamine from our food. HNMT is found in many tissues of our body, including the liver and the kidneys.
Because it is found throughout the body, HNMT plays a more significant role in degrading histamine that our bodies produces, such as from an allergic reaction.
Another enzyme that is often overlooked in the degradation of histamine is N-acetyltransferase 2 (NAT2).
The enzyme NAT2 acts as a “backup” system to degrade histamine that the body uses when histamine levels increase.
But NAT2 also breakdown many different chemicals and medications like sulfa antibiotics. Other substances that NAT2 breaks down or detoxifies are cigarette smoke, charring on grilled meat, caffeine, and some prescription medications.
Exposure to these chemicals or if you have a genetic variant that reduces the NAT2’s function; can increase the likelihood of being histamine intolerant.
Histamine toxicity results from too much histamine either from our food or being released that is not degraded correctly, reducing levels.
Some like to refer to your histamine bucket overflows leading to various symptoms like allergies, skin rashes, gastrointestinal disturbances, heartburn, headache, and autoimmune flare-ups.
We often focus too much on foods rich in histamine, but what can cause a high release of histamine? The chronic high release of histamine can lead to intolerance.
Some causes of chronic high levels of histamine release are environmental allergies, chronic mold infections, Lyme Disease, intestinal permeability (leaky gut), and long-term stress and anxiety.
What Can Affect the Levels of DAO and HNMT?
Many studies have shown that people who are struggling with histamine intolerance will have low serum (blood) levels of DAO. Current research shows that low levels of DAO are related to poor gut health, nutrient deficiencies, genetics, and medications.
Whereas most research on histamine intolerance is relatively recent, it has been shown that the number one symptom of histamine intolerance is gas, bloat, and IBS (constipation or diarrhea). These symptoms are all signs that you may have a leaky gut, poor digestion, malabsorption, and gut microbiota imbalances.
Most DAO is produced in the gut lining, dependent on a healthy gut microbiota (microbiome). A healthy and balanced gut microbiota helps to prevent leaky gut and increase DAO levels.
DAO is also dependent on many different nutrients, including copper, vitamin B2, B6, and vitamin C. Having deficiencies in any of these nutrients can lead to lower levels of DAO. Nutrient deficiencies can be due to poor diet, poor digestion, increased demand, and genetics.
Many medications, prescription and over-the-counter, can inhibit DAO and increase the release of histamine. Chronic use of some medications like Amitriptyline, a commonly prescribed antidepressant can lead to lower levels of DAO.
See my full list of medications that can impact histamine levels.
The enzyme HNMT is highly dependent on a process known as methylation, which depends on B vitamins, including choline. Methylation provides the compound S-adenosyl-L-methionine (SAMe) that allows HNMT to break down histamine found in our cells (intracellular).
If methylation is slowed down or not functioning optimally, this can lead to lower levels of HNMT. Nutrient deficiencies, chronic health conditions like mold infection, chronic stress, toxins, and poor gut health can all impact methylation and, therefore, levels of HNMT.
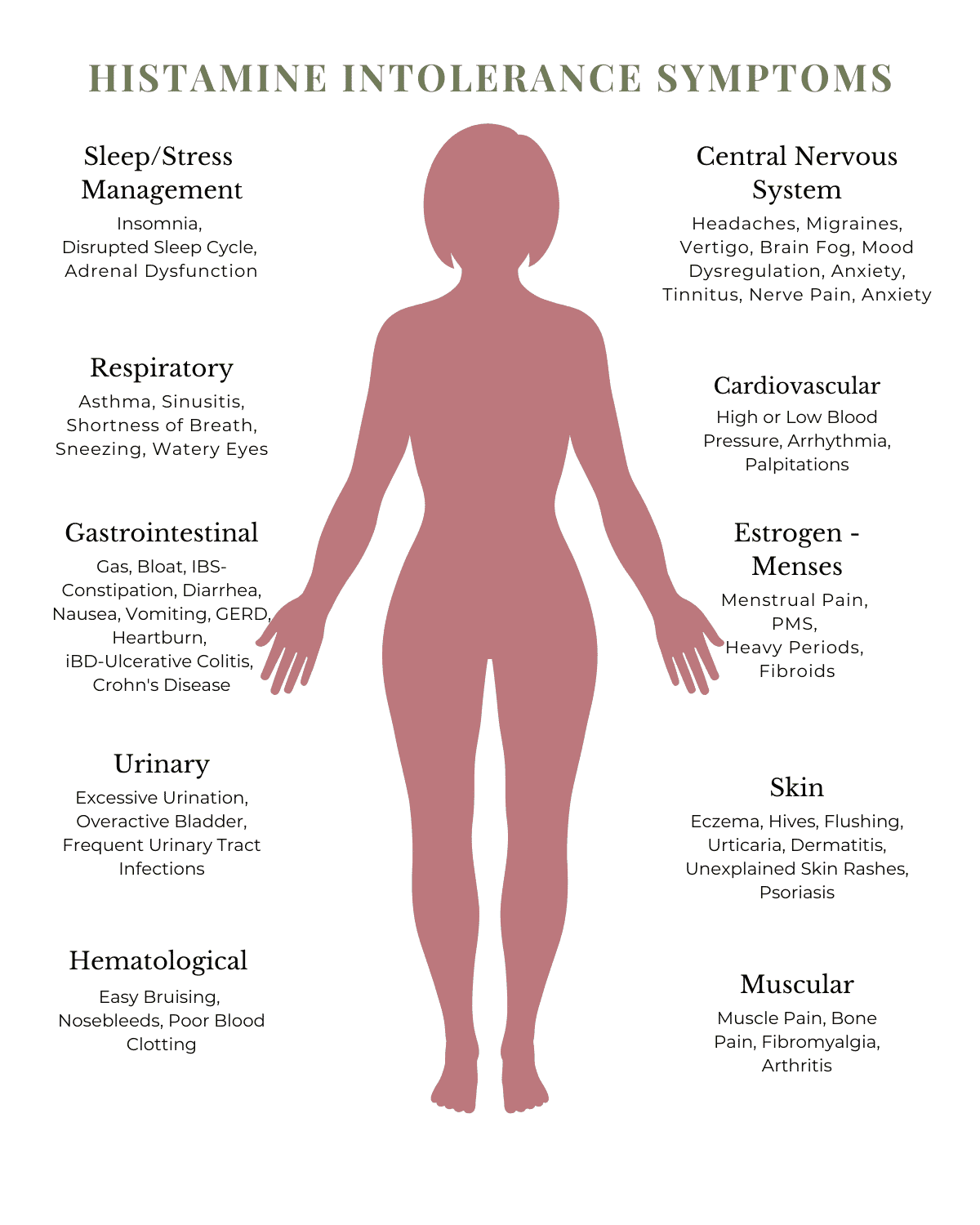
What are the Symptoms of Histamine Intolerance?
Histamine is synthesized and stored throughout our body to help perform many functions. One function is to support a healthy immune response to foreign invaders and act as an immune response when we have allergies.
When we develop allergies, we release high amounts of histamine hence the use of antihistamines to help control excessive histamine.
In addition, to providing a healthy immune response, histamine is used to promote the secretion of stomach acid. Most antacids block the action of histamine and are referred to as H2 blockers.
Because histamine is also produced as a neurotransmitter (brain signaling chemical), high histamine levels can impact our mental health and ability to sleep soundly throughout the night.
Histamine plays a critical role in our sleep/wake cycle and is regulated by melatonin. A deficiency in melatonin can lead to higher levels of histamine leading to waking up in the middle of the night and not being able to go back to sleep.
So, you can see how high histamine levels can lead to many symptoms, including digestive disturbances, insomnia, anxiety, and headaches.
What are The Causes of Histamine Intolerance?
Recent research shows that histamine intolerance originates in the gut, with the number one symptom being gas, bloat, and IBS. Maybe this is because the majority of dietary histamine is degraded or blocked by DAO, which is predominately produced in the gut lining.
Low levels of DAO were found in patients with irritable bowel disease (IBD), like ulcerative colitis and Crohn’s disease. By following a low histamine diet for four weeks, patients showed improvement in their symptoms.
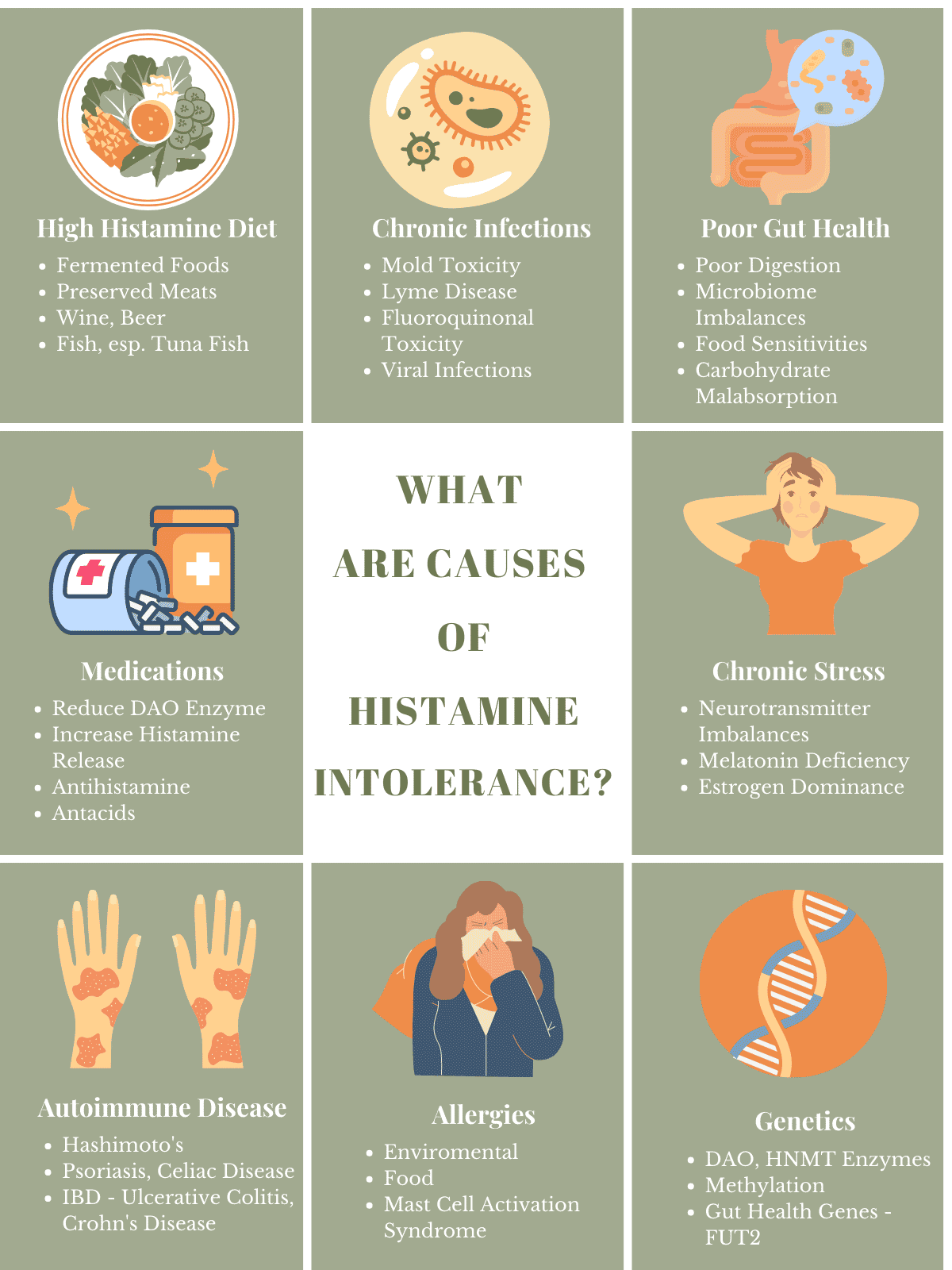
Whereas poor gut health is the number one cause of histamine intolerance, other causes are chronic stress, autoimmune conditions like psoriasis, medications, food sensitivities, and genetics.
Causes of Histamine Intolerances
What are the Genetics of Histamine Intolerance?
One of the steps to resolving histamine intolerance is to rule out your genetics. For me, genetic or genomics testing was a game changer when it came to overcoming my histamine intolerance. And, it has been for my clients too.
I would love to say that you could just test for your DAO genes and see if that is the reason why you struggle with histamine intolerance. Histamine intolerance is very polygenic, with numerous genes, including genes that involve nutrients like vitamin B6.
Even gut genes like the gene that is known as FUT2 can play a role in whether or not you might be more likely to develop histamine intolerance.
The best genetic report for histamine intolerance covers the enzymes (DAO, HNMT) and the nutrients genes like vitamin B6 that support DAO.
In addition, genes that play a role in methylation like MTHFR, would also give you what you would need to determine if you needed to support methylation to support the HNMT genes.
For me, the genes supporting methylation played the most significant role in my histamine intolerance.
And, why supplemental DAO enzymes didn’t work for me because I needed B vitamins to support HNMT rather than additional DAO.
How Do You Know if You are Histamine Intolerant?
Because symptoms of histamine intolerance are so varied, it can be challenging to determine if histamine intolerance is causing them.
In addition, other food intolerances can cause similar symptoms like lactose intolerance, glutamate intolerance, or sulfur intolerance. Even food sensitivities to nightshade vegetables (solanine) can have similar symptoms.
Lactose intolerance is the inability to digest the sugar found in non-fermented dairy products due to a lack of the enzyme lactase. It has been found that it is not uncommon to have both histamine and lactose intolerance.
Food sensitivities which are different food intolerances can also cause similar symptoms especially digestive disturbances, unexplained skin rashes, allergic-type reactions, and joint pain.
Currently, the gold standard test for histamine intolerance is to do a food/symptom journal for 30-day while staying on a low histamine diet. Get my food/journal for histamine, which includes a food list, and more.
Whereas there are no definitive tests for histamine intolerance, it has been found that testing for intestinal permeability marker known as zonulin, DAO and histamine blood levels is the best test. Not only does it test for histamine intolerance, it gets down the cause of your histamine intolerance.
The Advanced Intestinal Barrier Assessment by Precision Point is the test I use in my AIBA package to determine histamine intolerance and its cause.
See my blog for more information on the best test for histamine intolerance.
Advanced Intestinal Barrier Assessment Package
References:
1. Comas-Baste, et al, Histamine Intolerance: The Current State of the Art, Biomolecules, August, 2020
2. R Leintner, E Zoernpfenning, A Missbichler, Evaluation of the inhibitory effect of various drugs/active ingredients on the activity of human diamine oxidase in vitro
3. K Mori, C Maru, K Takasauna, K furuhama, Mechanism of histamine release induced by levofloxacin, a fluoroquinolone antibacterial agent, Eur J Pharacol, 2000, Apr 7
Eileen Schutte, MS, CN, FMN – One of my biggest passions is to help clients overcome food intolerances like histamine intolerance and sensitivities so that they can enjoy food again. My other passion is nutrigenomics, speaking to your genes through nutrition with focus on digestive health, autoimmune conditions, and skin health. I hold a master's degree in functional nutrition from the University of Bridgeport, Connecticut graduating Summa Cum Laude. After completing my masters I went on to get my certification in Functional Medicine Nutrition, and am a Certified LEAP Therapist (food sensitivities program). In addition, I am pursuing advanced education in Nutrigenomics through the American College of Nutrition.